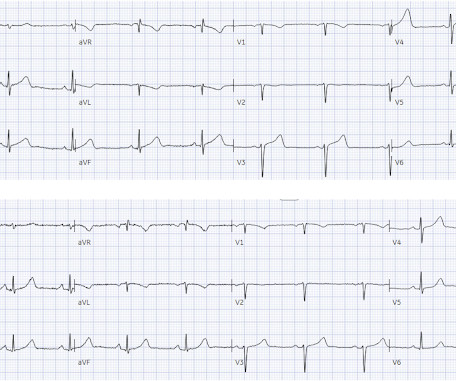
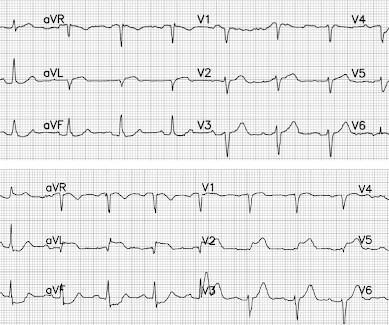
Guidelines would (erroneously) say that this patient who was defibrillated and resuscitated does not need emergent angiography
Dr. Smith's ECG Blog
JUNE 27, 2024
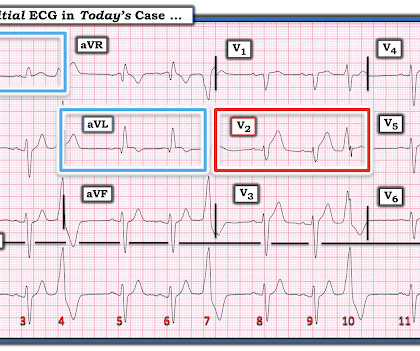
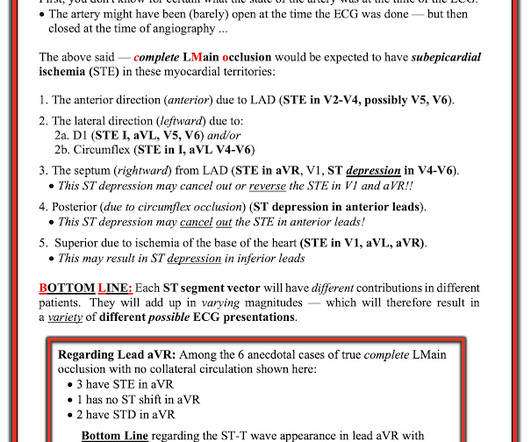
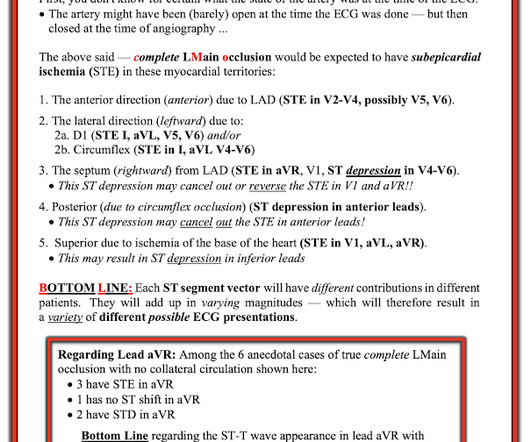
A patient had a cardiac arrest with ventricular fibrillation and was successfully defibrillated. The proof of this is that only 5% of patients enrolled had acute coronary occlusion. Coronary Angiography after Cardiac Arrest without ST-Segment Elevation. This study failed to do so. 5% vs. 58%!! As per Dr.











Let's personalize your content