ECG Cases 45 ECG in Weakness and Neurological Symptoms
Emergency Medicine Cases
SEPTEMBER 12, 2023
The post ECG Cases 45 ECG in Weakness and Neurological Symptoms appeared first on Emergency Medicine Cases.
This site uses cookies to improve your experience. To help us insure we adhere to various privacy regulations, please select your country/region of residence. If you do not select a country, we will assume you are from the United States. Select your Cookie Settings or view our Privacy Policy and Terms of Use.
Cookies and similar technologies are used on this website for proper function of the website, for tracking performance analytics and for marketing purposes. We and some of our third-party providers may use cookie data for various purposes. Please review the cookie settings below and choose your preference.
Used for the proper function of the website
Used for monitoring website traffic and interactions
Cookies and similar technologies are used on this website for proper function of the website, for tracking performance analytics and for marketing purposes. We and some of our third-party providers may use cookie data for various purposes. Please review the cookie settings below and choose your preference.
Emergency Medicine Cases
SEPTEMBER 12, 2023
The post ECG Cases 45 ECG in Weakness and Neurological Symptoms appeared first on Emergency Medicine Cases.
Dr. Smith's ECG Blog
SEPTEMBER 18, 2024
Compensatory enlargement was defined as being present when the total coronary arterial cross-sectional area at the stenotic site was greater than that at the proximal nonstenotic site. Thus, the lumen observed may actually still be the same size as the original, normal lumen. Unfortunately, vascular remodeling is variable and inconsistent.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.

Emergency Medicine Cases
FEBRUARY 28, 2023
Jesse McLaren on when to consider Spontaneous Coronary Artery Dissection (SCAD), which patients are at risk for reocclusion, and the challenges of diagnosing SCAD in patients who have nonischemic ECGs despite silent occlusion, occlusions perfused by collaterals, or from non-occlusive MI on this ECG Cases.
ACEP Now
DECEMBER 6, 2024
A 45-year-old male with a history of chronic obstructive pulmonary disease (COPD), asthma, amphetamine and tetrahydrocannabinol (THC) use, and coronary vasospasm presented to triage with chest pain. During assessment, the patient reported that a left heart catheterization six months prior indicated spasms but no coronary artery disease.

The Skeptics' Guide to EM
NOVEMBER 25, 2023
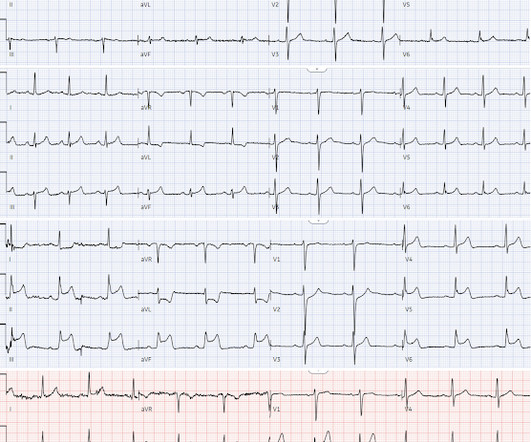
A 12-lead electrocardiogram (ECG) demonstrates ST elevations in leads II, III, and aVF with ST depressions in leads I and aVL and the team begins transport to the nearest percutaneous coronary intervention (PCI) capable hospital. Background: We have covered the issue of heart attacks several times on the SGEM. Reference: Stopyra et al.

EMS 12-Lead
APRIL 9, 2024
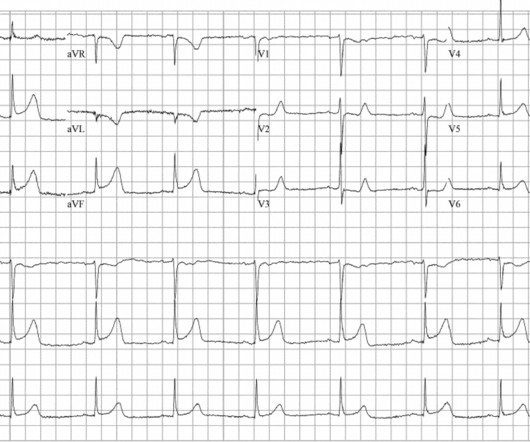
There is increased LV cavity dimensions with an increase in transient ischemic dilation, suggesting Left Main, or 3-vessel coronary artery disease. 2. Coronary angiography reveals significant and severe CAD involving all three epicardial vessels. He awoke earlier that morning in his usual state of health. Type I ischemia.
Emergency Medicine Cases
DECEMBER 16, 2019
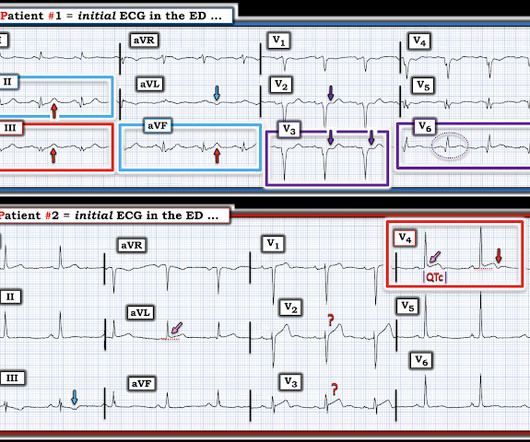
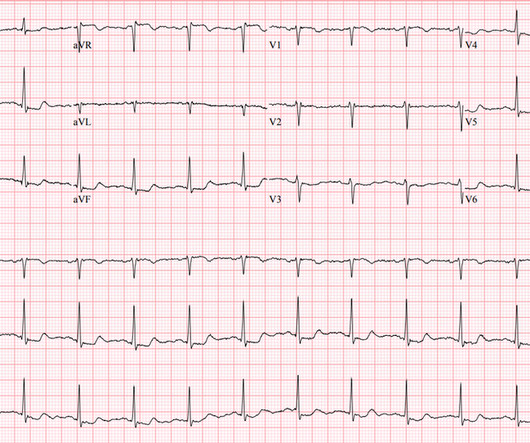
Which had acute coronary occlusion? In this ECG Cases blog we look at seven patients with potentially ischemic symptoms and subtle ECG changes in the lateral leads. Introducing the concept of Occlusion MI - a paradigm shift in ECG diagnosis of MI. The post ECG Cases 4: Lateral STEMI or Occlusion MI?
Dr. Smith's ECG Blog
NOVEMBER 15, 2023
Angiogram No obstructive epicardial coronary artery disease Cannot exclude non-ACS causes of troponin elevation including coronary vasospasm, stress cardiomyopathy, microvascular disease, etc. CORONARY ARTERIES: Exam was not directly tailored for coronary artery evaluation, noting recent diagnostic coronary angiogram.
Dr. Smith's ECG Blog
JANUARY 2, 2025
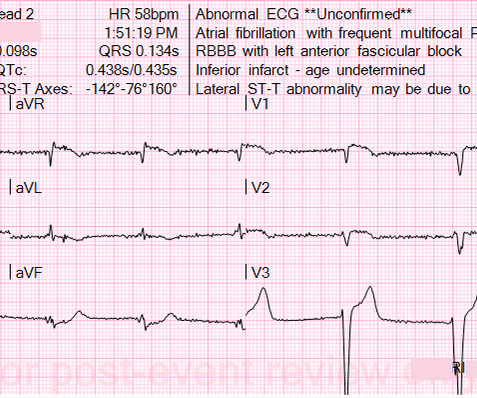
Among patients with left bundle branch block, T-wave peak to T-wave end time is prolonged in the presence of acute coronary occlusion. Finally, do a coronary angiogram Possible alternative to pacing is to give a beta-1 agonist to increase heart rate. T-waves are quite tall and possibly peaked (HyperK?), but potassium returned normal.
Dr. Smith's ECG Blog
DECEMBER 27, 2023
Note that as many as 7% of patients with acute coronary syndrome have chest pain reproducible on palpation [Lee, Solomon]. which reduces the pre-test probability of acute coronary syndrome by less than 30% [McGee]. Chest pain reproducible on palpation does not rule out acute coronary syndrome. Guagliumi, G., Iwaoka, R.

Emergency Medicine Cases
DECEMBER 20, 2023
ST/T changes: consider the differential including demand ischemia, associated electrolyte abnormalities, Brugada pattern from sodium channel blockade, and acute coronary occlusion vs vasospasm from cocaine. The post ECG Cases 47 – ECG Interpretation in Toxicology appeared first on Emergency Medicine Cases.
Dr. Smith's ECG Blog
OCTOBER 15, 2024
Additionally, his cardiac telemetry monitor showed runs of accelerated idioventricular rhythm, a benign arrhythmia often associated with coronary reperfusion. The patient is a 75-year old man with known coronary disease, including prior LAD and LCx OMI. That this patient has severe underlying coronary disease is indisputable.

The Skeptics' Guide to EM
JULY 2, 2022
Major adverse cardiac event rates in moderate-risk patients: Does prior coronary disease matter? Major adverse cardiac event rates in moderate-risk patients: Does prior coronary disease matter? He has no history of coronary artery disease. Date: June 30th, 2022 Reference: McGinnis et al. AEM June 2022. AEM June 2022.
First 10 EM
DECEMBER 25, 2023
Throughout the length of my career, we have consistently heard that less is more when it comes to blood transfusions (outside of the critically ill requiring massive transfusion, where the message, correct or not, has been the exact opposite).
Core EM
JANUARY 25, 2024
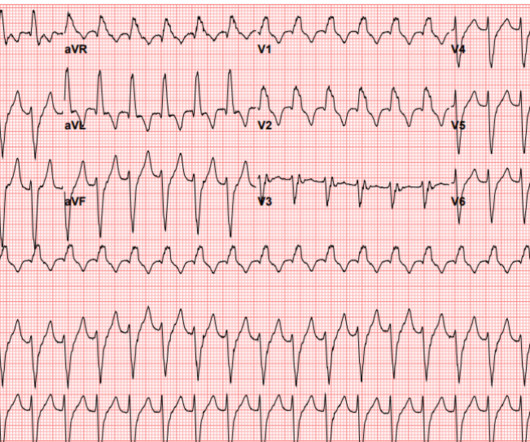
Risk factors that increase the likelihood of VT include history of previous myocardial infarction, known coronary artery disease, and structural heart disease. The differential diagnosis for this patient includes Ventricular Tachycardia (VT) and Supraventricular Tachycardia (SVT) with aberrancy. Sources [link] [link] [link] [link].
Dr. Smith's ECG Blog
OCTOBER 1, 2023
This patient in today's case was a man in his 60s with a known history of coronary disease, including prior stents. But in a patient with known coronary disease — who presents with new symptoms and the above ECG changes — any amount of Troponin elevation has to be taken as indicative of an acute event until proven otherwise.

ACEP Now
JULY 7, 2023
Extracorporeal membrane oxygenation Of patients with out-of-hospital cardiac arrest presenting to the ED in refractory VF, a majority have significant coronary artery disease, much of which is amenable to percutaneous coronary intervention. Out-of-hospital cardiac arrest is a commonly encountered entity in U.S.

EMDocs
NOVEMBER 6, 2023
Author: Brit Long, MD (@long_brit) // Reviewed by Alex Koyfman, MD (@EMHighAK) The American Heart Association 2023 Guideline for managing cardiac arrest or life-threatening toxicity due to poisoning was recently released. This post will focus on the key parts of the guideline that affect ED evaluation and management. Top 10 Take Home Pearls 1.

Dr. Smith's ECG Blog
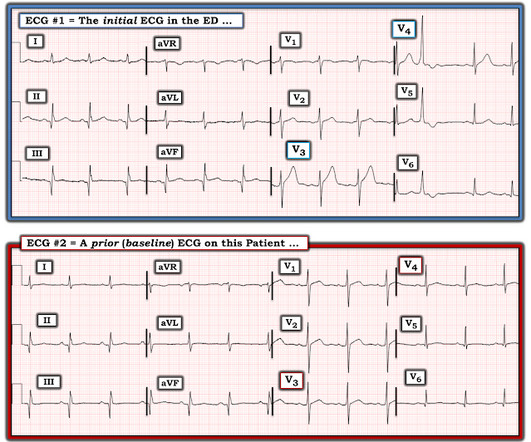
SEPTEMBER 22, 2023
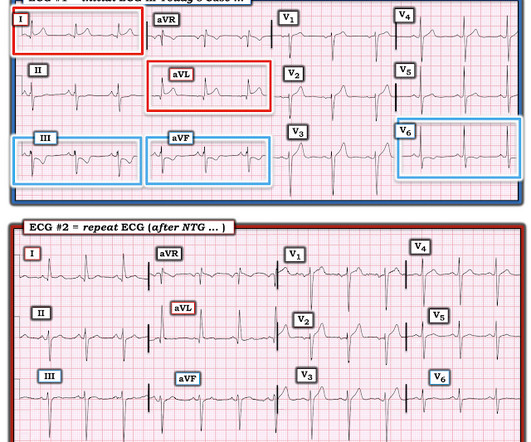
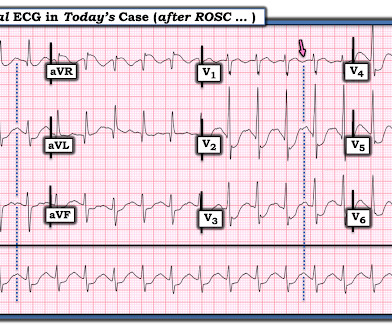
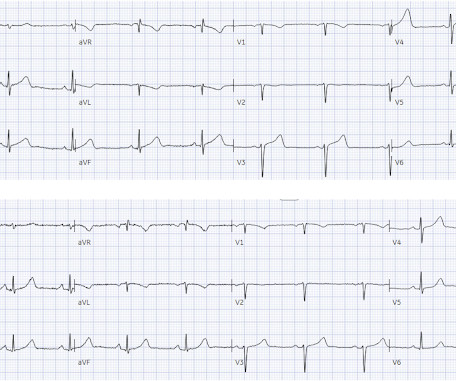
This is diagnostic of full reperfusion.] An old ECG was found: As you can see, this patient has zero baseline STE, and normal T-waves. You never know if a patient's baseline has normal large STE or complete absence of STE, or somewhere in between. 90% of normals have some STE in V2 and V3. I focus my comment on this initial ECG in today's case.
Dr. Smith's ECG Blog
JUNE 5, 2024
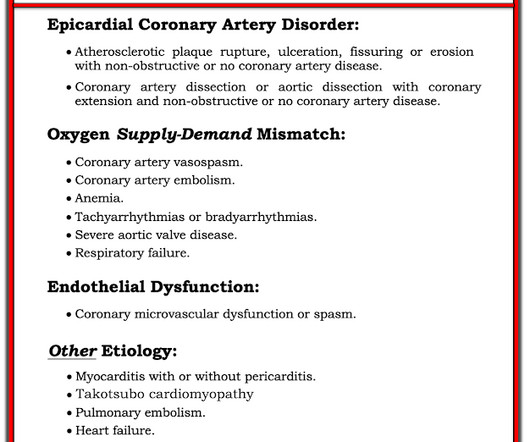
Why Was Cardiac Cath Negative for Coronary Disease? As noted by Dr. Nossen — this patient qualified as MINOCA ( M yocardial I nfarction with N on- O bstructive C oronary A rteries ) — since troponin was positive on his 2nd admission, yet there was no evidence of obstructive coronary disease on cath.
EMS 12-Lead
JULY 24, 2023
Category 1 : Sudden narrowing of a coronary artery due to ACS (plaque rupture with thrombosis and/or downstream showering of platelet-fibrin aggregates. It’s judicious, then, to arrange for coronary angiogram. Supply-demand mismatch (non-occlusive coronary disease, or exacerbation of preexisting flow insufficiency) a.
Dr. Smith's ECG Blog
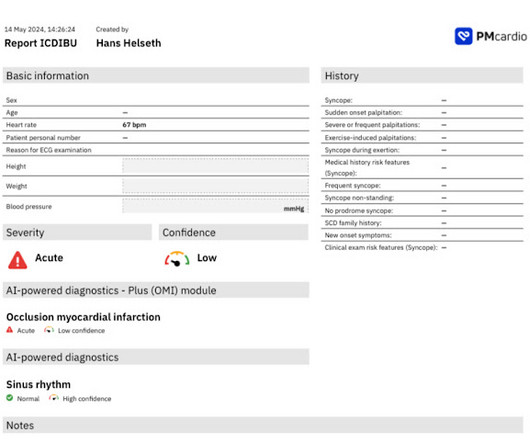
MARCH 10, 2025
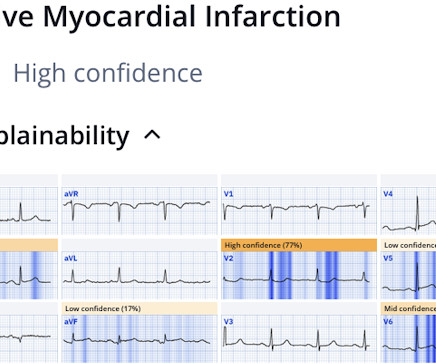
But like many similar studies, the study was small (one year at one centre with no indication of the incidence of acute coronary occlusion), and it used as the gold standard the final cardiologist interpretation of the ECG - not the patient outcome! So waiting for serial troponin would have further delayed reperfusion. Take home 1.
Dr. Smith's ECG Blog
JULY 25, 2024
But cardiac arrest is a period of near zero flow in the coronary arteries and causes SEVERE ischemia. Smith's ECG Blog ( See My Comment in the March 1, 2023 post) — DSI does not indicate acute coronary occlusion! It also does not uniformly indicate severe coronary disease. The ECG shows severe ischemia, possibly posterior OMI.
Dr. Smith's ECG Blog
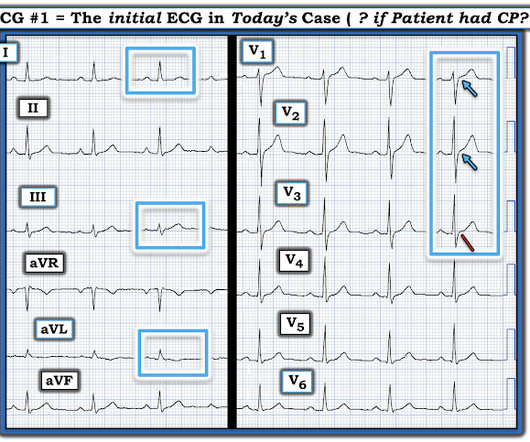
AUGUST 6, 2023
Doing so allows you to put YOURSELF to the TEST ( keeping in mind that all ECGs shown are from patients with chest pain suggestive of potential acute coronary disease ). Smith shows a new ECG. So — FREEZE the picture of each ECG on the screen — FORCE yourself to commit to an answer.

The Skeptics' Guide to EM
JANUARY 18, 2020
Date: January 16th, 2020 Reference: Troponin Testing and Coronary Syndrome in Geriatric Patients With Nonspecific Complaints: Are We Overtesting? Date: January 16th, 2020 Reference: Troponin Testing and Coronary Syndrome in Geriatric Patients With Nonspecific Complaints: Are We Overtesting?
EMS 12-Lead
SEPTEMBER 6, 2022
Coronary thrombosis is a dynamic process of platelet aggregation and subsequent coagulation. During spontaneous reperfusion -- whether via thrombolysis, or recruitment of collateral circulation -- there exists characteristic ST/T changes on the ECG. Case Review: [link]

Dr. Smith's ECG Blog
NOVEMBER 29, 2023
This new ECG was still interpreted as STEMI and the patient was taken to the cath lab where the angiogram showed completely normal coronary arteries throughout. Smith : this ECG is definitely not OMI, but could be mistaken for Swirl pattern, which is a septal OMI with STE in V1 and STD in V6. Unfortunately no echo was available.

The Skeptics' Guide to EM
SEPTEMBER 11, 2021
Acute coronary syndrome (ACS) is responsible for the majority (60%) of all OHCAs in patients. Emergency coronary angiography is reasonable for select (eg, electrically or hemodynamically unstable) adult patients who are comatose after OHCA of suspected cardiac origin but without ST elevation on ECG (Class IIa, LOE B-NR).
Emergency Medicine Cases
SEPTEMBER 15, 2020
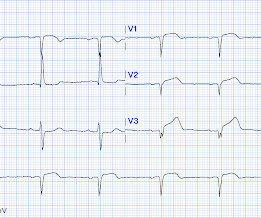
Which had an acute coronary occlusion? Signs of occlusion MI in patients with LVH include: new Q waves/loss of R waves, disproportionate and dynamic ST elevation (or ST depression from posterior MI), and hyperacute T waves. In this ECG Cases blog we look at 6 patients who presented with potentially ischemic symptoms and LVH on their ECG.

EMS 12-Lead
SEPTEMBER 5, 2022
Another spurious finding is a QS pattern that mimics Anterior MI, and in the acute setting this may elicit compulsory urge to pursue invasive coronary intervention that is entirely unwarranted. Tom Bouthillet demonstrates appropriate electrode application when capturing the pre-hospital 12 Lead ECG: [link]
Dr. Smith's ECG Blog
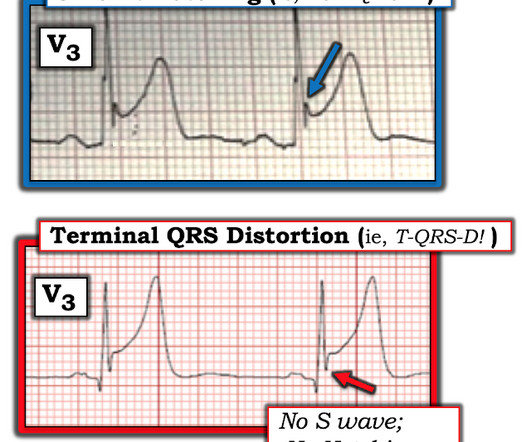
OCTOBER 8, 2024
In the context of this woman in her 60s who has known coronary disease ( and who is now presenting with acute chest discomfort ) — I interpreted neighboring leads V1 and V2 as part of the same acute process suggested by the QRST in lead V3.
EMS 12-Lead
MAY 20, 2022
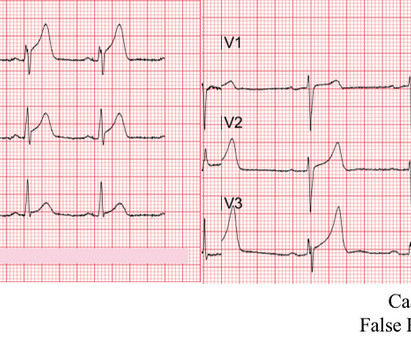
Additional architectural changes include systolic anterior motion of the mitral valve, endothelial dysfunction at the level of the coronary arterial bed, and ventricular diastolic dysfunction. This worried the crew of potential acute coronary syndrome and STEMI was activated pre-hospital. It is spread to V2 and V3.

EMDocs
DECEMBER 11, 2023
Emergency physicians have recognized for some time that there are many occlusions of the coronary arteries that do not present with classic STEMI criteria on the ECG. This included the addition several new STEMI equivalents [4] on ECG that warrant “prompt evaluation for emergency coronary angiography.”
Dr. Smith's ECG Blog
DECEMBER 7, 2023
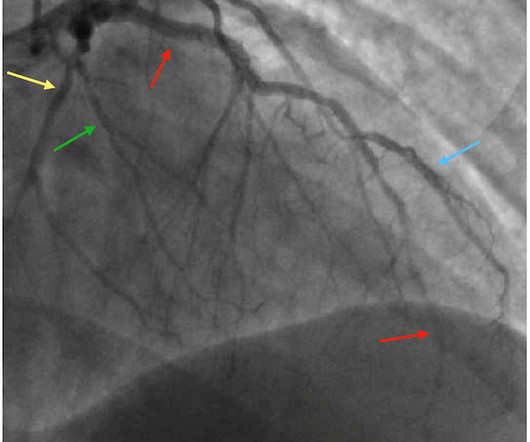
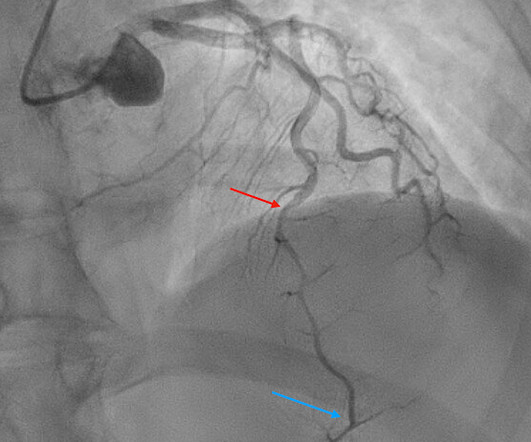
I quickly reviewed the patient’s records and saw that she was a 53 year old woman with a history of BMI 40, but no other identifiable risk factors for coronary artery disease. In this patient with stuttering symptoms and rising troponin, there is no other option but to perform emergent coronary angiography. Hers is shown below.
Dr. Smith's ECG Blog
DECEMBER 19, 2023
The commonest causes of MINOCA include: atherosclerotic causes such as plaque rupture or erosion with spontaneous thrombolysis, and non-atherosclerotic causes such as coronary vasospasm (sometimes called variant angina or Prinzmetal's angina), coronary embolism or thrombosis, possibly microvascular dysfunction. This is not the case.

EMS 12-Lead
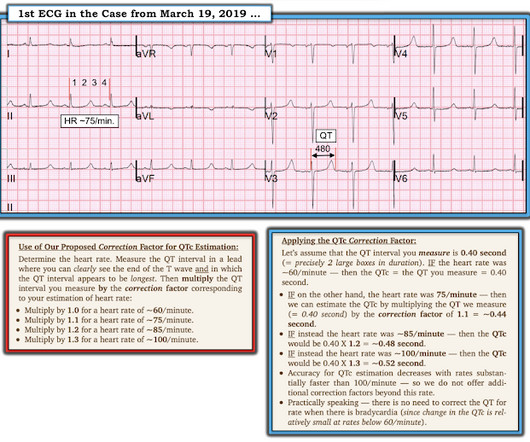
MARCH 19, 2023
He denied any known medical history, specifically: coronary artery disease, hypertension, dyslipidemia, diabetes, heart failure, myocardial infarction, or any prior PCI/stent. Learning points 1] Acute Coronary Syndrome has many shades of clinical manifestation. Breath sounds were clear in all lung fields. No appreciable skin pallor.

Dr. Smith's ECG Blog
APRIL 18, 2024
The ECG is just a test: a Bayesian approach to acute coronary occlusion If a patient with a recent femur fracture has sudden onset of pleuritic chest pain, shortness of breath, and hemoptysis, the D-dimer doesn’t matter: the patient’s pre-test likelihood for PE is so high that they need a CT. But does this matter?
Dr. Smith's ECG Blog
SEPTEMBER 25, 2024
Here is the post shock ECG: Cardiology was called stat for ischemic VT, query SCAD vs thrombotic occlusion vs coronary vasospasm. Cath lab was activated: There was no coronary artery disease, but there was spontaneous coronary artery dissection (SCAD) of the distal LAD, which was narrowed by 95%, and treated medically.
EMS 12-Lead
JUNE 20, 2022
One cannot rely on this feature as a means of detecting changes – subtle, or dramatic – for volatile occlusive coronary thrombus. Discussion When the QRS is normal, is the encountered ST/T changes that beget suspicion for LAD ACS (as in both of these cases) the result of occlusive coronary thrombus, or simply a normal variant?
Dr. Smith's ECG Blog
MAY 20, 2024
The scan also showed “scattered coronary artery plaques”. __ Smith comment 1 : the appropriate management at this point is to lower the blood pressure (lower afterload, which increases myocardial oxygen demand). They too have dense white masses consistent with coronary atherosclerosis. The blue circle shows the LCx.
REBEL EM
OCTOBER 25, 2023
Take Home Points: A CCTA is an anatomic test to determine if a patient has normal coronary arteries, non-obstructive disease, or obstructive disease. Take Home Points: A CCTA is an anatomic test to determine if a patient has normal coronary arteries, non-obstructive disease, or obstructive disease.
Dr. Smith's ECG Blog
JUNE 7, 2024
The most likely would be #2) initially normal, then #3) subtle OMI, then #4) obvious STEMI, and then #1) reperfusion: In other words, the patient with an initially normal ECG develops an acute coronary occlusion, with ECGs that progress from subtle to obvious, and then reperfuse after angiography. 2 Normal ECG #3.

Dr. Smith's ECG Blog
APRIL 9, 2024
Before the lab values returned this patient had a n emergent coronary CT angiogram done that ruled out CAD. A false positive cath lab activation is also off course acceptable for this diagnosis if you cannot get an emergent coronary CT angiogram. Each main coronary artery (LAD, RCA and LCx) are shown in separate images.

EMDocs
JANUARY 8, 2024
Emergent coronary angiography is not recommended over a delayed or selective strategy in patients with ROSC after cardiac arrest in the absence of ST-segment elevation, shock, electrical instability, signs of significant myocardial damage, and ongoing ischemia (Level 3: no benefit). COR 2a, LOE B-R. COR 2a, LOE C-LD. COR 2b, LOE B-R.
Expert insights. Personalized for you.
We have resent the email to
Are you sure you want to cancel your subscriptions?


Let's personalize your content